Abstract

TRIO has been shown to be associate with higher risk of morbidity (infections, venocclusive disease and hepatic dysfunction) and mortality after allogeneic HCT. A high transplant iron score (>25 red cell unit transfused prior to HCT, serum ferritin > 1000 ng/ml and a bone marrow (BM) iron stain of +6) was associated with 50% decrease in survival at one year (Storey J. Hem & Oncol 2009). TRIO in BM macrophages can generate free radicals resulting in oxidant stress thereby altering the hematopoietic microenvironment. This could have adverse effects on hematopoiesis and affect engraftment after HCT. To date, limited data are available on the effect of TRIO on outcomes of UCB HCT. We examined whether TRIO quantified based on serum ferritin (sF) and BM iron score (MIS) impact outcomes of UCB HCT, particularly with regards to engraftment.
We reviewed 150 consecutive patients (pts) who underwent UCB HCT between March 2006 and September 2015 at City of Hope. Median age at time of HCT was 33.5 years (yrs) (range: 0-70 years) with 55% male and 23% < 18 yrs of age. sF was available within 30 days before HCT for 65%, and MIS was assessed on the pre-HCT BM biopsy for 40% of pts. HCT indications included bone marrow failure (n=13), hemoglobinopathies (n=2), lymphoma (n=23), acute leukemia (n=104), and chronic leukemia (n=8). Disease risk index (DRI) was high/very-high in 38% and 20% of pts had HCT comorbidity index of more than 2. One cord graft was received for 20% of pts. Median TNC of 4.9X10^7/kg (range: 1.8-26.6) and median CD34 count of 1.8X10^5/kg (range: 0.2-122.4). HLA match status was 4/6, 5/6, 6/6 in 93, 48, and 9 pts. Almost 60% of pts received myeloablative conditioning regimen (MAC) and 80% had calcineurin inhibitor/mycophenolate mofetil for graft versus host disease (GVHD) prophylaxis.
With a median follow-up of 48.1 months (range: 5.8- 119.6), 2- and 5-yrs progression free survival (PFS) were 41% and 35.5% while 2- and 5-yrs OS were 47% and 36%, respectively. Cumulative incidence (CI) of NRM at 2 and 5 yrs were 35.7 and 40.6% and CI of relapse at 2- and 5-yrs were 23 and 24%, respectively. Day 100 grade II-IV and grade III/IV aGvHD were 56.7% and 28.7%. 2 yrs CI of cGvHD was 51.7% with 38.8% extensive cGvHD. DRI was found to be significant factor for relapse (HR 1.74 95%CI 0.88-3.45 p<0.001) and conditioning regimen significantly affect OS (HR= 1.92 95%CI 1.24-2.96; p=0.003), PFS (HR= 2.12 CI 1.39-3.24; p<0.001) and relapse rate (HR= 4.07 CI 1.95-8.49; p<0.001) when non-myeloablative/reduced intensity conditioning was compared with MAC. However, day 100 grade II-IV and III/IV aGVHD was increased in pts with MAC (65.1% vs 45.3%; p=0.006 and 37.2% vs 17.2%; p=0.005; respectively) with no significant effect seen on the NRM (p=0.9).
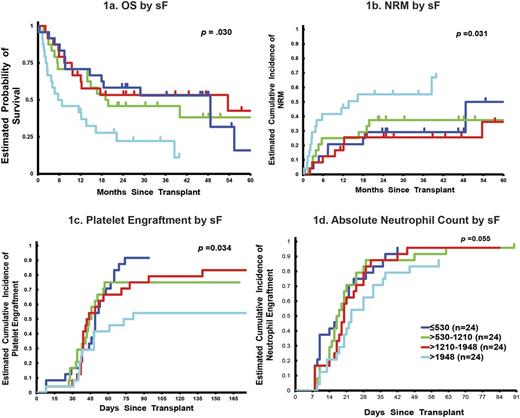
In multivariable analysis, sF <1000 ng/ml independently predicted for shorter OS (HR=0.49; CI 0.27-0.88 p=0.015). When the impact of sF was examined by quartiles, pts in the highest sF quartile (>1948 ng/ml) had shorter OS (HR=3.05, 95%CI: 1.40-6.66; p=0.03) and higher NRM (HR=2.79, 95%CI: 1.16-6.72; p=0.03) compared to those in the lowest quartile (<530 ng/ml) (Fig 1a and b). There was no statistically significant difference in regards to disease relapse, or incidence of acute or chronic GVHD across sF groups.
Patients in the highest sF quartile had delayed platelet engraftment compared to those in the lowest quartile (HR=0.46, 95%CI: 0.24-0.89, p=0.03). A trend towards delayed neutrophil engraftment was also observed between these 2 groups (HR=0.57, 95%CI: 0.33-0.99; p=0.055) (Fig 1c and d). No significant difference was seen in neutrophil (p=0.67) or platelet engraftment (p=0.92) based on MIS. But there was a statistically significant increase of grade II-IV aGVHD in pts with MIS of 3-4 (63.8% vs 30.8% at day 100; p=0.04). This however did not translate into worse OS, NRM or relapse.
In conclusion, TRIO measured by sF has an adverse impact on OS and NRM in recipients of UCB HCT. Elevated sF is also associated with delay in platelet and neutrophil engraftment after UCB HCT. MIS was not associated with time to engraftment, however, this value was available in only 40% of pts. Therefore, TRIO should be considered as a risk factor for adverse outcome and poor graft function after UCB HCT.
Nademanee: seattle Genetics: Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal